In a scientific advancement that carries profound implications for global reproductive medicine, researchers in the United Kingdom have successfully pioneered the use of three-parent In Vitro Fertilization (IVF) techniques to help prevent the transmission of mitochondrial diseases from mother to child. More than 60 babies have reportedly been born globally using this cutting-edge technique, with the first confirmed births in the UK bringing renewed medical and ethical discussions to the forefront.
This development is trending not only in Europe but also in India, where discussions around IVF, genetic diseases, and assisted reproduction are frequent in both medical and public discourse. Many Indian health professionals are observing this breakthrough closely, acknowledging its potential to benefit families afflicted by incurable hereditary illnesses while debating its ethical, societal, and religious ramifications.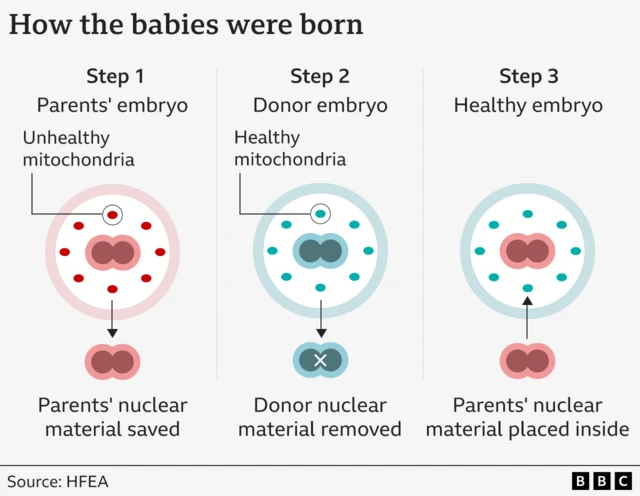
What Is Mitochondrial Disease and Why It Matters
Mitochondria, often described as the “powerhouses” of the cell, are tiny structures within each cell responsible for generating energy. They are inherited exclusively from the mother, and mutations in mitochondrial DNA can lead to a range of conditions that affect the brain, heart, muscles, and vital organ functions. These diseases can be fatal and are generally incurable, making prevention the only reliable option for families at risk.
In India, though awareness remains low, thousands of cases go undiagnosed or misdiagnosed every year, particularly among children showing neurological, muscular, or developmental symptoms. With current medical treatments only able to manage symptoms, the possibility of eliminating these mutations during conception offers the hope of erasing some forms of genetic suffering within a generation.
The Three-Parent IVF Technique Demystified
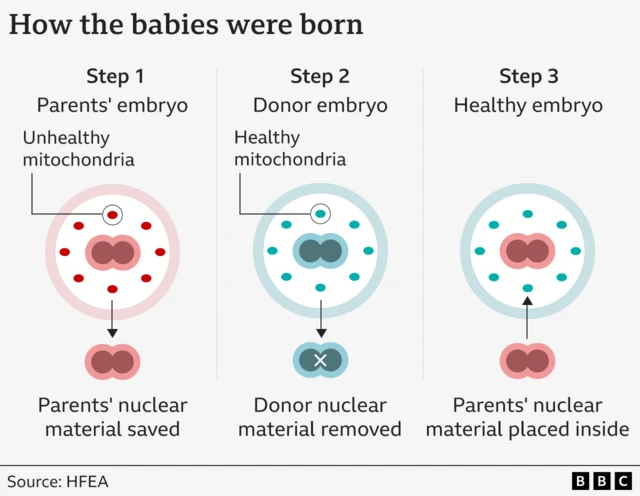
The three-parent IVF process, also known as Mitochondrial Donation Therapy (MDT) or Mitochondrial Replacement Therapy (MRT), involves the combination of genetic material from three individuals:
-
Mother – provides the nucleus from her egg, which contains 99.8% of her DNA.
-
Father – provides sperm, contributing no mitochondrial DNA.
-
Donor Woman – provides an egg with healthy mitochondria but without the nucleus.
The mother’s nucleus is extracted and inserted into the donor egg (which has had its nucleus removed), creating a hybrid egg with the mother’s nuclear DNA and the donor’s healthy mitochondrial DNA. This egg is then fertilized with the father’s sperm and implanted into the mother through standard IVF procedures.
The child born this way inherits nuclear DNA from their parents, which determines appearance and personality traits, and only mitochondrial DNA from the donor, which affects cell energy but not identity traits. Therefore, the term “three-parent baby” is scientific in basis but misleading emotionally, as the donor’s genetic impact is limited to just 0.2% of total DNA.
First Confirmed UK Births and Scientific Oversight
The United Kingdom became the first country to approve mitochondrial donation legally in 2015 under tightly regulated medical conditions. The treatment is offered only through licensed IVF clinics on a case-by-case basis, and only families with a high risk of passing on serious mitochondrial illnesses qualify.
In 2023, a British fertility center successfully delivered the first babies born through the technique, and more recent reports confirm the procedure has now resulted in a handful of live births with no signs of mitochondrial conditions recurring in children. These babies are under specialist health monitoring to track long-term outcomes and developmental progress. Results so far have been encouraging and highly optimistic, providing a foundation for potential openness in countries like India.
Ethical Concerns and Religious Sensitivities
With every scientific leap forward, there are layers of ethical and emotional complexity, especially on technologies that alter core biological processes like reproduction. Critics of three-parent IVF raise numerous questions: Is it ethical to “design” a baby through modified genetics? Are we tampering with nature in ways that might have future unforeseen consequences?
Some religious groups view the process as interfering with “divine intent”, while others worry it could lead to so-called “designer babies”, where parents eventually begin choosing traits beyond health, such as height, intelligence, or looks. However, so far, mitochondrial donation is only permitted to prevent life-threatening diseases, not cosmetic alteration or enhancement.
In India, societies deeply rooted in familial traditions are divided on assisted reproduction and IVF in general, often leading to social stigma. Still, perspectives are changing. As infertility rates climb and awareness spreads, especially in urban and semi-urban populations, such technologies are slowly gaining acceptance.

Relevance and Future Potential for India
In India, more than 27 million couples reportedly suffer from infertility, and around 20,000 children are born with mitochondrial disorders every year, many of whom don’t survive beyond adolescence. For parents carrying these recessive mutations, the only alternative until now was avoiding biological pregnancy entirely or hoping against odds.
With global success stories growing, the Indian Council of Medical Research (ICMR) is reviewing the potential merits and feasibility of adapting regulated mitochondrial donation procedures within India’s IVF ecosystem. Pilot research centers may be launched in partnership with advanced genetic labs, paving the way for further clinical trials down the line.
If enabled here under proper oversight, thousands of families could soon benefit from this technology, especially women who previously had no safe way to pass on their genetic legacy without risk.
Medical Community’s Response and Readiness
Doctors and fertility specialists in India are cautiously optimistic. While excited by the prospect of preventing degenerative conditions in children, many stress the need for clear regulations, consent protocols, and robust post-natal monitoring. Some fear misuse in unregulated IVF labs or misrepresentation of the treatment as a “beautify-your-baby” technique by unscrupulous clinics.
India’s fertility market is still recovering from challenges like improper embryo storage, multiple implantation malpractice, and high legal costs. Therefore, introducing mitochondrial replacement would require a dedicated legal and ethical framework, widespread medical training, and centralized audits.
Still, doctors agree that technology aimed solely at reducing suffering—within medically controlled boundaries—should not be dismissed due to philosophical bias. “Preventing irreversible genetic illness in children should qualify as a human right,” remarks one leading fertility expert.
Cost and Accessibility: Can India Afford It?
One of the biggest barriers in bringing mitochondrial therapy to India is cost. In the UK, a single case of mitochondrial IVF can cost more than ₹30-40 lakh (approx. £30,000 – £40,000) when considering donor cycles, extraction, fertilization, and post-birth monitoring. For most Indian families, this figure is unthinkable.
However, with India’s burgeoning medical tourism and emerging biotech hubs, localized protocols could reduce unit costs significantly. If government funding or insurance partnerships are built into the framework, select high-risk patients may be able to access subsidized treatment.
Private hospitals in metros like Delhi, Mumbai, Hyderabad, and Bengaluru are already equipped with advanced embryology labs capable of handling the complex stages of nuclear transfer—should the ethical green light be given in the coming years.

Public Awareness and Media Influence
Public reception of three-parent IVF in the UK has been cautiously positive. As media portrayals grow more nuanced and understanding of mitochondrial disease increases, more families are entering consultation phases. In India too, news of such global advancements quickly goes viral across platforms—fueling interest, fear, and debate in equal measure.
Social media conversations have ranged from curiosity (“Can this help save babies born with incurable diseases?”) to philosophical trepidation (“Are we crossing lines that shouldn’t be crossed?”). Some influencers and parenting accounts are already explaining the concept in regional languages, helping break down scientific ideas into relatable stories.
In this way, public discourse is helping normalize conversations around genetic illness, reproductive rights, and emerging medicine—an essential step before any nationwide roll-out can occur.
Safeguards and the Way Forward
Introducing such a sensitive technology in a socio-culturally diverse country like India will require meticulous planning. Consent laws must be robust, families need thorough counseling, and regulatory bodies will have to carry out frequent audits of clinics that might one day perform mitochondrial therapy.
Experts suggest setting up an independent Bioethics Review Committee composed of doctors, ethicists, lawyers, and civic representatives to oversee developments in this space. Public consultations, media literacy campaigns, and patient support systems will all be crucial in ensuring that the benefits of this procedure are shared responsibly and fairly.
Conclusion: A New Chapter in Safe, Healthy Parenthood
The birth of babies using three-parent IVF is more than just medical news—it’s a powerful reminder of how far science has come in protecting families from inherited suffering. For couples carrying damaging mutations, especially mothers with mitochondrial DNA faults, this development offers the chance to enjoy the miracle of biological parenthood without passing on disease.
In India, where genetics-related birth defects and family planning challenges intersect, the arrival of such a game-changing solution might still be years away—but the conversation has started. And in that conversation lies hope: for mothers, for children yet to be born, and for a healthcare system slowly making its way toward the future.
This paradigm-shifting advancement in reproductive technology, now showcased by the UK’s pioneering efforts, prompts Indian families, healthcare professionals, and policymakers to realistically consider a future where the heartbreak of passing on incurable mitochondrial diseases could become a thing of the past—ushering in new hope for healthier generations while urging society to thoughtfully weigh the promise and responsibility that come with rewriting the rules of human inheritance.
Follow: Mitochondrial Diseases
Also Read: Shocking Twists as Kannada Star Ranya Rao Gets 1-Year Jail in ₹12.5 Crore Gold Smuggling Scandal

